How AI is Transforming Medical Billing: Key Benefits & Use Cases
- February 18, 2025
-
3004 Views
- by Ishan Vyas

Medical billing is an essential part of revenue cycle management(RCM) in the healthcare industry. It ensures accurate and timely payment for services offered by healthcare providers. This complicated process involves coding, claims, posting, and denial management. However, these traditional medical billing systems are fraught with inefficiencies, such as coding errors, delayed claims, and administrative bottlenecks. Such issues not only create cash flow problems but also lead to significant revenue loss problems, making the effective billing of healthcare a real challenge.
The entire process has significantly become more efficient and effective in the healthcare sector with the integration of artificial intelligence. The overall benefits that such integration brings are transformative to the sector. A report by Mordor Intelligence estimated that the AI in Medical Billing market was expected to rise from $4.49 billion in 2025 to $12.65 billion by 2030 at a CAGR of 23.01% during the forecast period of 2025-2030.
Impact of AI in Medical Billing
1. Enhanced Medical Coding Accuracy
By using machine learning (ML) and natural language processing (NLP) in healthcare, artificial intelligence (AI) greatly improves the accuracy of medical coding.To assign the proper medical billing codes (like ICD-10 and CPT), these tools examine a patient’s medical records, including clinical notes, diagnosis, treatment information, and procedures. Through the analysis of these unstructured documents, AI reduces errors and improves coding consistency by rapidly matching the correct codes with little assistance from humans.
For example, AI-powered coding tools examine medical records and perform auto-encoding of appropriate diagnostic and procedure codes. It frees healthcare professionals from human errors frequently resulting in rejections and also helps in quick submission of error-free claims without delay. This system alleviates the coder workload, leaving him or her the opportunity to do more challenging ones and leave more routine ones for AI.
How AI Assists:
- Automated Code Assignment: To assign precise codes, AI systems employ natural language processing (NLP) to evaluate and interpret lab results, medical histories, and doctor’s notes.
- Enhances Compliance: AI makes sure that medical codes follow rules and industry standards, avoiding misclassification and lowering the possibility of audits or legal problems.
- Enhances Learning: AI-based coding systems are constantly learning from data and patterns, which helps them become more accurate over time and adjust to changing medical procedures and codes.
2. Faster and Easier Processing of Claims
Due to manual data entry, validation, and submission, claim processing in the healthcare industry is most often slower and error-prone. AI speeds up and improves the accuracy of this process by automating the verification of payer-specific rules, diagnosis codes, and patient data. The time spent examining, revising, and resubmitting claims is greatly decreased by automated claim submission systems, which results in a quicker and more efficient revenue cycle.
How AI Assists:
- Quicker Claim Approvals: This reduces the time for claim submission and minimizes the delays that arise from manual procedures.
- Error Reduction: The software identifies and corrects errors before claims are submitted, hence minimizing rejections.
- Cost Efficiency: This reduces costs since there is minimal need for manual labor and rework on denied claims, hence strengthening AI medical coding software development.
- Improved Compliance: AI for medical billing ensures compliance with insurance regulations and guidelines, thereby reducing legal risks.
3. Denial Management
Artificial intelligence improves denial management through denial trend analysis and root cause identification behind claim rejections. It helps in developing effective strategies to address these issues so that resubmissions can be done faster and approvals take place much sooner. AI can also prioritize high-value claims for resolution and provide actionable insights toward prevention of future denials, thus gradually improving the overall success rate of claims.
How AI Assists:
- Faster Resolution: Speedy identification of issues and redressal of denied claims issues.
- Root Cause Analysis: Identifies repeat errors and trends in claim denials.
- Enhanced Approval Rate: Increases the chances of a successful resubmission of the claim.
- Proactive Prevention: Suggests process improvements that will minimize future denials.
4. Cost Reduction Through Automation
Eligibility verification, payment posting, and account reconciliation are examples of manual medical billing tasks that can be expensive and time-consuming. By automating repetitive tasks, AI helps to streamline these administrative procedures. This lowers operating costs for healthcare providers by enabling them to hire fewer employees to perform such duties. AI-driven automation also guarantees that tasks are finished more quickly and precisely, preventing expensive errors and enhancing the practice’s overall financial performance..
How AI Assists:
- Automates Repetitive processes: AI takes care of repetitive processes like eligibility verification and payment posting, freeing up resources to concentrate on more strategic billing elements.
- Lowers Administrative Costs: AI lowers the need for manual labour by automating critical procedures, which lowers overhead costs.
- Boosts Efficiency: AI systems are more efficient than humans, finishing jobs faster and more accurately while also enhancing cash flow and cutting down on delays.
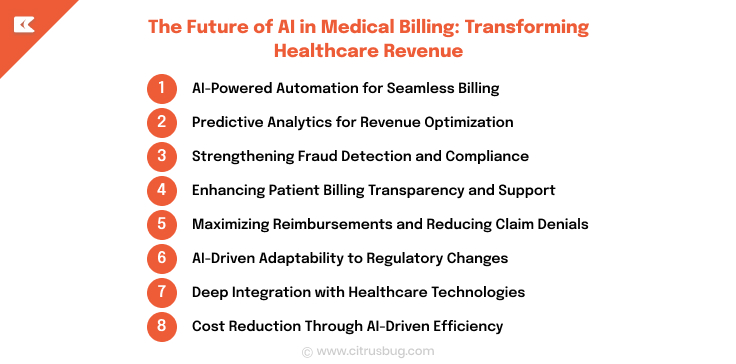
The Future of AI in Medical Billing: Transforming Healthcare Revenue
As AI continues to evolve, its impact on medical billing is becoming more profound. From automating workflows to enhancing financial forecasting and fraud detection, AI-driven solutions are reshaping how healthcare organizations manage billing and revenue cycles. Here’s a look at the key advancements that will define the future of AI in medical billing.
1. AI-Powered Automation for Seamless Billing
AI is revolutionizing medical billing by automating tasks across the entire billing lifecycle from patient registration to claim processing and payment posting. This reduces human intervention, minimizes errors, and accelerates revenue collection.
- Automated Data Processing: AI will extract, verify, and manage patient data with minimal manual effort, reducing administrative burdens.
- Integrated Billing Systems: By synchronizing with electronic health records (EHRs) and billing software, AI ensures accurate, real-time claim submissions.
2. Predictive Analytics for Revenue Optimization
AI’s ability to analyze vast datasets enables healthcare providers to predict revenue trends and proactively optimize their billing strategies.
- Revenue Forecasting: AI will assess historical billing data, payer patterns, and seasonal trends to anticipate fluctuations in cash flow.
- Strategic Adjustments: With predictive insights, providers can optimize collections, resource allocation, and staffing to maintain financial stability.
3. Strengthening Fraud Detection and Compliance
Medical billing fraud and coding errors can result in financial losses and regulatory issues. AI-driven fraud detection systems identify anomalies and flag suspicious activities in real-time.
- Anomaly Detection: Machine learning models continuously analyze billing data to detect inconsistencies such as overbilling or upcoding.
- Instant Alerts: AI will notify billing departments of irregularities, enabling quick intervention and compliance with industry regulations.
4. Enhancing Patient Billing Transparency and Support
One of the biggest challenges in medical billing is the lack of transparency for patients. AI solutions improve billing clarity and offer personalized support.
- Real-Time Billing Updates: Patients receive automated notifications about outstanding balances, insurance coverage, and payment deadlines.
- AI-Powered Assistance: Virtual assistants and chatbots provide instant responses to billing inquiries, simplifying the payment process.
5. Maximizing Reimbursements and Reducing Claim Denials
AI will refine the claims process to minimize errors and improve reimbursement rates, ensuring healthcare providers receive timely payments.
- Error-Free Claims Submission: AI will flag undercoding, missing documentation, and other issues before claims are submitted.
- Adaptive Billing Strategies: AI continuously learns from payer behaviors, adjusting claim submissions to align with evolving billing requirements.
6. AI-Driven Adaptability to Regulatory Changes
With frequent updates to medical codes and payer policies, AI-powered billing systems will ensure seamless compliance.
- Automated Compliance Updates: AI keeps billing systems aligned with the latest regulations, reducing the risk of penalties.
- Continuous Learning: AI refines billing accuracy over time by learning from claim patterns and industry trends.
7. Deep Integration with Healthcare Technologies
AI will bridge the gap between medical billing and other healthcare technologies, creating a connected ecosystem.
- EHR and EMR Integration: AI-powered billing systems will extract relevant patient data from electronic health records for precise claim coding.
- AI in Diagnostics & Billing: Billing AI will correlate diagnosis data with medical procedures to validate charges and reduce disputes.
8. Cost Reduction Through AI-Driven Efficiency
AI will significantly cut administrative costs by optimizing workflows, reducing manual errors, and minimizing claim rejections.
- Streamlined Workflows: AI-driven automation reduces the need for extensive billing teams, lowering operational expenses.
- Fewer Rejected Claims: With improved accuracy, AI will reduce claim denials, saving time and financial resources.
Conclusion: The Role of AI in Medical Billing Software Development
The integration of AI in medical billing is transforming revenue cycle management by automating workflows, enhancing accuracy, and reducing inefficiencies. From predictive analytics and fraud detection to claim optimization and regulatory compliance, AI-driven solutions are addressing long-standing challenges in medical billing.
For such healthcare software development, this evolution presents a significant opportunity. AI-powered billing software can streamline the entire billing cycle, ensuring faster reimbursements, minimizing errors, and reducing operational costs. Developers must focus on building intelligent, scalable, and adaptive billing systems that seamlessly integrate with electronic health records (EHRs) and payer networks.
For over a decade now, Citrusbug has been offering end-to-end medical billing software development services to various surgical centers, healthcare organizations, and private practices. To complete your medical billing cycle prior to the submission date, our experts employ multi-level quality check systems and advanced technology-based processes. We also remain updated with changing medical billing laws and regulations and ensure complete compliance with state, federal, and payer requirements. Contact us today and enhance your medical billing processes along with a strong focus on superior patient care.




 SaaS Development
SaaS Development Web Application Development
Web Application Development Mobile Application Development
Mobile Application Development Custom Software Development
Custom Software Development Cloud Development
Cloud Development DevOps Development
DevOps Development MVP Development
MVP Development Digital Product Development
Digital Product Development Hire Chatbot Developers
Hire Chatbot Developers Hire Python Developers
Hire Python Developers Hire Django Developers
Hire Django Developers Hire ReactJS Developers
Hire ReactJS Developers Hire AngularJS Developers
Hire AngularJS Developers Hire VueJS Developers
Hire VueJS Developers Hire Full Stack Developers
Hire Full Stack Developers Hire Back End Developers
Hire Back End Developers Hire Front End Developers
Hire Front End Developers AI Healthcare Software Development & Consulting
AI Healthcare Software Development & Consulting Healthcare App Development
Healthcare App Development EHR Software Development
EHR Software Development Healthcare AI Chatbot Development
Healthcare AI Chatbot Development Telemedicine App Development Company
Telemedicine App Development Company Medical Billing Software Development
Medical Billing Software Development Fitness App Development
Fitness App Development RPM Software Development
RPM Software Development Medicine Delivery App Development
Medicine Delivery App Development Medical Device Software Development
Medical Device Software Development Patient Engagement Software Solutions
Patient Engagement Software Solutions Mental Health App Development
Mental Health App Development Healthcare IT Consulting
Healthcare IT Consulting Healthcare CRM Software Development
Healthcare CRM Software Development Healthcare IT Managed Services
Healthcare IT Managed Services Healthcare Software Testing services
Healthcare Software Testing services Medical Practice Management Software
Medical Practice Management Software Outsourcing Healthcare IT Services
Outsourcing Healthcare IT Services IoT Solutions for Healthcare
IoT Solutions for Healthcare Medical Image Analysis Software Development Services
Medical Image Analysis Software Development Services Lending Software Development Services
Lending Software Development Services Payment Gateway Software Development
Payment Gateway Software Development Accounting Software Development
Accounting Software Development AI-Driven Banking App Development
AI-Driven Banking App Development Insurance Software Development
Insurance Software Development Finance Software Development
Finance Software Development Loan Management Software Development
Loan Management Software Development Decentralized Finance Development Services
Decentralized Finance Development Services eWallet App Development
eWallet App Development Payment App Development
Payment App Development Money Transfer App Development
Money Transfer App Development Mortgage Software Development
Mortgage Software Development Insurance Fraud Detection Software Development
Insurance Fraud Detection Software Development Wealth Management Software Development
Wealth Management Software Development Cryptocurrency Exchange Platform Development
Cryptocurrency Exchange Platform Development Neobank App Development
Neobank App Development Stock Trading App Development
Stock Trading App Development AML software Development
AML software Development Web3 Wallet Development
Web3 Wallet Development Robo-Advisor App Development
Robo-Advisor App Development Supply Chain Management Software Development
Supply Chain Management Software Development Fleet Management Software Development
Fleet Management Software Development Warehouse Management Software Development
Warehouse Management Software Development LMS Development
LMS Development Education App Development
Education App Development Inventory Management Software Development
Inventory Management Software Development Property Management Software Development
Property Management Software Development Real Estate CRM Software Development
Real Estate CRM Software Development Real Estate Document Management Software
Real Estate Document Management Software Construction App Development
Construction App Development Construction ERP Software Development
Construction ERP Software Development