How AI and Automation Are Enhancing EHR Functionality?
- June 30, 2025
-
2023 Views
- by Ishan Vyas
Table of Contents
- What are Electronic Health Records (EHRs)?
- The Role of AI in Elevating EHR Performance
- Automation in EHR: Removing Friction From Healthcare Workflows
- AI-Powered Features in Modern EHR Platforms
- Real-Life Workflow Enhancements With AI in EHR
- Challenges in Integrating AI into EHR Systems
- How to Build an AI-Ready EHR System: A Step-by-Step Approach
- Conclusion: Smarter EHRs Start With AI

In the past, Electronic Health Records (EHRs) served solely to keep databases of patients’ information. However, in this modern era of medicine, doing just that is not sufficient. What healthcare professionals require goes beyond having their records digitally saved; they need systems that aid them in decision-making, support error avoidance, and save time.
Nowadays, EHRs are integrating AI and automation technologies to address these requirements. These advanced features come with embedded predictive insights, natural language processing capabilities, and automated task flows. Intelligent systems are rapidly becoming the new norm for patient care as more providers begin adopting custom EHR software development services.
What are Electronic Health Records (EHRs)?
Electronic Health Records (EHRs) are digital versions of a patient’s medical history, health details, and treatment records. Patients, treating physicians, and doctors can all quickly access these records. The transition from antiquated paper-based systems to digital formats, such as AI-driven EHR, offers many benefits to AI in healthcare.
AI-powered EHR systems can also automate a lot of administrative work. They are able to identify trends in patient data and warn medical practitioners of possible dangers. This improves patient care even more and raises the healthcare system’s general effectiveness.
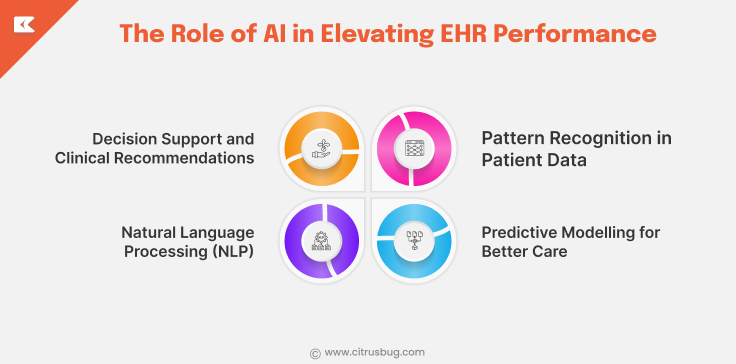
The Role of AI in Elevating EHR Performance
The way EHR systems function is being redefined by artificial intelligence. Modern platforms employ AI in EHR to assist with data analysis, risk identification, and real-time clinical decision support, as opposed to serving as passive databases. As a result of this change, EHRs are becoming more than just tools for keeping records; they are becoming actively involved in providing care.
Here are the key ways AI is improving EHR systems:
1. Pattern Recognition in Patient Data
AI can quickly scan through large volumes of patient records to identify trends and red flags. For example:
- Recognizing early signs of chronic conditions
- Detecting abnormal lab results
- Highlighting medication interactions
This supports faster diagnosis and more personalized treatment planning.
2. Predictive Modeling for Better Care
AI algorithms can forecast future health risks based on a patient’s history, lifestyle, and current symptoms. This includes:
- Predicting hospital readmission risks
- Forecasting potential complications after surgery
- Identifying patients who may benefit from early intervention
Such predictive tools are central to many AI use cases in healthcare, helping teams shift from reactive to proactive care.
3. Natural Language Processing (NLP)
Most clinical data exists in free-text doctors’ notes, discharge summaries, and reports. NLP helps:
- Extract key information from unstructured text
- Auto-fill structured fields in the EHR to build a patient profile.
- Improve the accuracy of patient records without extra manual work.
This reduces time spent on documentation and increases data usability.
4. Decision Support and Clinical Recommendations
AI-driven decision support systems (CDSS) use data to suggest relevant actions during patient care, such as:
- Recommended diagnostic tests
- Evidence-based treatment options
- Alerts about potentially unsafe prescriptions
These systems assist, not replace, clinical judgment, making care safer and more consistent.
AI enhances EHR performance by improving data interpretation, predicting risks, reducing documentation burden, and supporting informed decisions at every step.
Automation in EHR: Removing Friction From Healthcare Workflows
Automation plays a vital role in strengthening the impact of artificial intelligence in EHR platforms. While AI handles the intelligent decision-making side, automation focuses on reducing repetitive manual work, freeing up healthcare professionals to focus on direct patient care and enabling the compliance automation solution to handle regulatory checks seamlessly.
Automated scripts push lab orders, flag overdue vaccines, and remix visit notes into patient-friendly language while clerks and clinicians tend to pressing matters at the bedside. Below are some of the most valuable ways automation is improving everyday EHR workflows.
1. Patient Onboarding and Scheduling Become Seamless
Signing in a new patient and lining up their first visit can eat up a surprising amount of time in a packed clinic. Automation takes a lot of that busywork out of the picture by:
- Gathering basic info with a quick, secure online form.
- Double-checking insurance details before anyone walks through the door.
- Finding openings that actually line up with the patients schedule.
- Shooting out a text or e-mail reminder so appointments arent suddenly forgotten.
These automated steps help reduce administrative effort while improving the patient experience.
2. Medical Billing and Coding Are Less Error-Prone
Manual billing frequently introduces errors, spurs claim denials, and delays the payment cycle. By shifting to an automated platform, providers can stabilize the revenue stream through:
- Assigning correct diagnosis and procedure codes based on documentation
- Checking for missing or incorrect data before claim submission
- Flagging billing issues in real-time for staff review
The result is fewer denials and faster reimbursement cycles. According to HealthIT.gov, automating billing within EHRs has significantly improved the financial performance of many healthcare practices.
3. Real-Time Alerts Improve Response Time
One of the biggest advantages of EHR automation is how quickly it can trigger alerts based on real-time data. For example, when critical lab results are posted, the system can:
- Instantly notify the assigned physician
- Send reminders to nurses for follow-up
- Log the action in the patient record automatically
These kinds of trigger-based actions reduce delays and make sure that important steps in care are never missed.
4. Discharge and Follow-Up Are Better Coordinated
Automation helps hospitals and clinics handle discharges more effectively by generating patient-specific instructions and ensuring proper follow-up. Once a patient is cleared to go home, the system can:
- Auto-fill discharge summaries with personalized care instructions
- Schedule lab tests or follow-up appointments
- Send reminders and educational content via SMS or email
- Update the patient’s EHR with all post-care activities
By combining automation with AI in EHR workflows, healthcare organizations are not only saving time, they’re also improving care quality and operational consistency.
This not only supports continuity of care but also reduces the chances of readmission. For long-term gains, many healthcare organizations now invest in custom-built EHR systems tailored to their discharge and care coordination workflows.
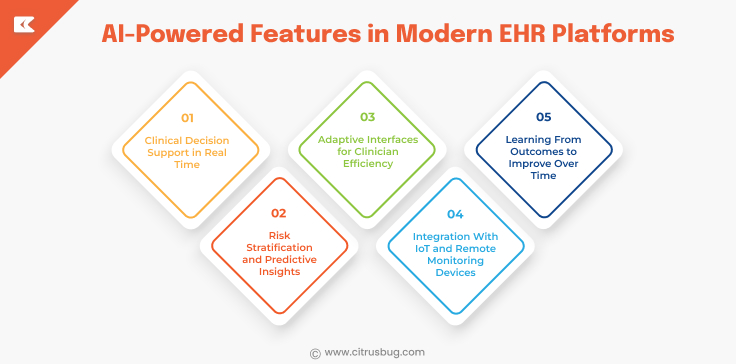
AI-Powered Features in Modern EHR Platforms
Artificial intelligence is no longer just a “nice to have” in healthcare; it’s becoming essential to how EHR systems operate. Modern EHR platforms are being upgraded with AI features that support clinical decisions, reduce administrative tasks, and make healthcare data more useful in real time.
Let’s look at some of the key AI-powered capabilities transforming today’s EHR systems:
1. Clinical Decision Support in Real Time
One of the most impactful applications of AI is assisting doctors with real-time suggestions during patient care. AI can analyse a patient’s history, lab results, and symptoms to offer:
- Recommended diagnostic tests
- Treatment options based on clinical guidelines
- Alerts for high-risk prescriptions or allergies
These decision support tools help clinicians act faster and avoid potential mistakes.
2. Risk Stratification and Predictive Insights
AI models can assess the likelihood of complications, disease progression, or readmission. These insights are invaluable for:
- Identifying patients who may need preventive care
- Managing chronic conditions more effectively
- Reducing unnecessary hospitalisations
Hospitals are using these predictive tools to improve outcomes and reduce costs across patient populations.
A research article published in JAMA highlights how machine learning integrated into EHRs has helped predict sepsis hours before it occurs, proving the real-world impact of such tools.
3. Adaptive Interfaces for Clinician Efficiency
AI can personalize the EHR interface based on each clinician’s behaviour and workflow preferences. This results in:
- Fewer clicks to access frequently used data
- Smarter auto-fill options based on past entries
- A smoother, more intuitive user experience
By learning from user habits, the system becomes easier to navigate and less frustrating for busy healthcare providers.
4. Integration With IoT and Remote Monitoring Devices
Modern EHRs often pull real-time data from wearables, home monitoring devices, and in-hospital equipment. AI helps:
- Filter meaningful patterns from continuous data streams
- Trigger alerts when metrics cross unsafe thresholds
- Present summaries within the EHR for easy review
This feature supports remote patient monitoring, especially for chronic care programs.
5. Learning From Outcomes to Improve Over Time
Some AI-powered EHRs are designed to learn from past treatment outcomes. By tracking what worked for similar patients in the past, they can:
- Suggest adjustments to care plans
- Refine the clinical pathway
- Support evidence-based decision-making
This type of ongoing learning makes the system more innovative and more useful the more it’s used.
As demand grows for personalized care and more intelligent workflows, many providers are turning to healthcare software development agency that can build and integrate these intelligent features within their existing platforms.
Real-Life Workflow Enhancements With AI in EHR
When applied to routine healthcare workflows, AI’s actual value in EHR systems becomes apparent. Improving the real-time collaboration of physicians, nurses, and administrative personnel is more important than focusing only on technology. Artificial intelligence is improving the speed, intelligence, and dependability of EHR systems from patient intake to discharge.
Let’s take a look at what workflows used to look like and how intelligent EHR systems are changing them for the better.
Before: Documentation Was Time-Consuming and Error-Prone
Clinicians often spent 20–30% of their time entering or correcting patient information. Notes were incomplete, and errors were common especially when systems didn’t flag them in real time.
Now: AI Helps Capture Clean, Complete Records
NLP and smart prompts now assist with documentation. The system suggests missing entries, flags inconsistencies, and even fills fields automatically based on context. This leads to higher data accuracy and less time wasted on revisions.
Before: Manual Follow-Ups and Missed Appointments
Staff had to manually call patients, confirm appointments, and schedule follow-ups, tasks prone to delays and human oversight.
Now: Automated Scheduling and Communication
EHRs integrated with automation tools now handle this behind the scenes. Appointment reminders, follow-up scheduling, and post-visit surveys are sent automatically, improving patient compliance and saving hours each week.
Before: Critical Information Was Hard to Find
Important updates like test results or medication changes were buried in charts or missed during handovers, leading to poor coordination.
Now: Real-Time Alerts and Workflow Triggers
AI flags priority updates and routes them to the proper care team member instantly. Everyone stays informed, and most importantly, urgent issues are addressed without delay.
Before: Teams Worked in Silos
Different departments used disconnected systems, resulting in gaps, duplicated work, and delays in patient care.
Now: EHRs Support Connected, Collaborative Care
AI-enhanced EHRs now support task automation, progress tracking, and centralized updates helping teams collaborate better. Many healthcare providers are now building custom EHR platforms to support their unique workflows end-to-end.
Challenges in Integrating AI into EHR Systems
While the advantages of AI technology in EHR systems are obvious, the journey to effective integration isn’t always a smooth one. Most healthcare organizations encounter problems with data quality AI tools require structured, comprehensive data, but legacy systems contain broken or dirty records. Without clean data, even the most intelligent algorithms fail to produce accurate insights.
Another universal obstacle is interoperability. EHR systems normally operate within silos, and it is difficult for AI models to consume and analyze data between systems. This reduces their impact and puts more pressure on expert healthcare IT consulting to bridge these systems.
Trust from clinicians is also an issue. If an AI suggestion is not transparent, physicians will be reluctant to use it. That’s why effective AI in EHR systems needs to be explainable and have smooth workflows so they feel like a natural extension of the care process rather than a disruption.
Lastly, privacy laws such as HIPAA demand stringent protection for any system that utilizes patient information. AI systems need to adhere to best security practices, access controls, and audit trail tracking to remain compliant and trustworthy.
How to Build an AI-Ready EHR System: A Step-by-Step Approach
Bringing AI in EHR systems to life takes more than plugging in an algorithm. It requires the right foundation, the right use cases, and the right team. Here’s how healthcare organizations can build an EHR system ready for artificial intelligence:
Step 1: Start with Clean, Standardized Data
AI models depend on accurate, structured data to generate useful results. Before integrating AI, focus on:
- Eliminating duplicate or inconsistent entries
- Standardizing formats across departments
- Using HL7/FHIR protocols to support interoperability
Without reliable data, AI in EHR systems can’t function effectively.
Step 2: Define Real-World Use Cases First
Don’t adopt AI just for the sake of innovation. Instead, look for specific pain points in your workflow, like slow diagnosis, manual charting, or high readmission rates. Then, map AI to those issues.
Start small:
- Use AI for clinical documentation support
- Implement predictive alerts for high-risk patients
- Automate routine admin processes
Each use case should offer visible value to care teams.
Step 3: Build a User-Centric Interface
AI features should blend into existing workflows, not disrupt them. A successful EHR interface:
- Makes suggestions without overwhelming the user
- Explains “why” behind each AI-driven recommendation
- Allows clinicians to override or give feedback
This builds trust and drives long-term adoption.
Step 4: Ensure Compliance and Data Security
With AI accessing sensitive health data, compliance is critical. Your platform must be HIPAA-compliant and offer:
- Role-based access
- Detailed audit logs
- Data encryption both at rest and in transit
If you’re not sure where to begin, working with experienced healthcare AI software development consultants can help speed up development while staying compliant.
Step 5: Build for Scalability
Even if you begin small, architect the system so it can handle future use cases. Whether you decide to add voice input, merge wearables, or utilise NLP to uncover clinical insights, your architecture should expand as your requirements grow.
Conclusion: Smarter EHRs Start With AI
As healthcare becomes increasingly data-driven and personalized, the use of AI within EHR systems is gaining foundational status. From automating administrative functions and streamlining processes to providing predictive information and enhancing documentation, AI is enabling EHRs to transition from passive recordkeeping mechanisms to smart clinical assistants.
But success doesn’t happen by accident. It requires clean data, careful design, easy-to-use features, and strategic deployment. Whether you’re replacing an outdated platform or beginning from scratch, working with the right healthcare IT professionals can enable you to create a smarter, future-proofed EHR system that actually empowers care teams and patients to collaborate and thrive.




 SaaS Development
SaaS Development Web Application Development
Web Application Development Mobile Application Development
Mobile Application Development Custom Software Development
Custom Software Development Cloud Development
Cloud Development DevOps Development
DevOps Development MVP Development
MVP Development Digital Product Development
Digital Product Development Hire Chatbot Developers
Hire Chatbot Developers Hire Python Developers
Hire Python Developers Hire Django Developers
Hire Django Developers Hire ReactJS Developers
Hire ReactJS Developers Hire AngularJS Developers
Hire AngularJS Developers Hire VueJS Developers
Hire VueJS Developers Hire Full Stack Developers
Hire Full Stack Developers Hire Back End Developers
Hire Back End Developers Hire Front End Developers
Hire Front End Developers AI Healthcare Software Development & Consulting
AI Healthcare Software Development & Consulting Healthcare App Development
Healthcare App Development EHR Software Development
EHR Software Development Healthcare AI Chatbot Development
Healthcare AI Chatbot Development Telemedicine App Development Company
Telemedicine App Development Company Medical Billing Software Development
Medical Billing Software Development Fitness App Development
Fitness App Development RPM Software Development
RPM Software Development Medicine Delivery App Development
Medicine Delivery App Development Medical Device Software Development
Medical Device Software Development Patient Engagement Software Solutions
Patient Engagement Software Solutions Mental Health App Development
Mental Health App Development Healthcare IT Consulting
Healthcare IT Consulting Healthcare CRM Software Development
Healthcare CRM Software Development Healthcare IT Managed Services
Healthcare IT Managed Services Healthcare Software Testing services
Healthcare Software Testing services Medical Practice Management Software
Medical Practice Management Software Outsourcing Healthcare IT Services
Outsourcing Healthcare IT Services IoT Solutions for Healthcare
IoT Solutions for Healthcare Medical Image Analysis Software Development Services
Medical Image Analysis Software Development Services Lending Software Development Services
Lending Software Development Services Payment Gateway Software Development
Payment Gateway Software Development Accounting Software Development
Accounting Software Development AI-Driven Banking App Development
AI-Driven Banking App Development Insurance Software Development
Insurance Software Development Finance Software Development
Finance Software Development Loan Management Software Development
Loan Management Software Development Decentralized Finance Development Services
Decentralized Finance Development Services eWallet App Development
eWallet App Development Payment App Development
Payment App Development Money Transfer App Development
Money Transfer App Development Mortgage Software Development
Mortgage Software Development Insurance Fraud Detection Software Development
Insurance Fraud Detection Software Development Wealth Management Software Development
Wealth Management Software Development Cryptocurrency Exchange Platform Development
Cryptocurrency Exchange Platform Development Neobank App Development
Neobank App Development Stock Trading App Development
Stock Trading App Development AML software Development
AML software Development Web3 Wallet Development
Web3 Wallet Development Robo-Advisor App Development
Robo-Advisor App Development Supply Chain Management Software Development
Supply Chain Management Software Development Fleet Management Software Development
Fleet Management Software Development Warehouse Management Software Development
Warehouse Management Software Development LMS Development
LMS Development Education App Development
Education App Development Inventory Management Software Development
Inventory Management Software Development Property Management Software Development
Property Management Software Development Real Estate CRM Software Development
Real Estate CRM Software Development Real Estate Document Management Software
Real Estate Document Management Software Construction App Development
Construction App Development Construction ERP Software Development
Construction ERP Software Development