Accredited Healthcare Software Development Company By
Key Features and Benefits of Healthcare Claim Management Software
-
Claim Validation
Verify claims before submitting them to decrease errors and rejections. This improves accuracy, lowers denial rates, and expedites the reimbursement period with health insurance.
-
Automated Coding
Utilize AI-based coding to make claims preparation easier. This reduces the amount of work required manually, reduces costs associated with administration, and ensures adherence to coding standards.
-
Payer Integration
Connect directly with payer systems for smooth data exchange. This minimizes delays, improves communication, and helps providers get reimbursed faster.
-
Denial Management
Track, analyze, and resolve denied claims quickly. This helps recover lost revenue and reduces recurring mistakes in future claim submissions.
-
Analytics and Reporting
Access detailed reports and insights in real time. This allows healthcare organizations to identify bottlenecks, improve decision-making, and enhance overall financial performance.
-
Payment and Remittance Management
Automate payment posting and reconciliation with ease. This improves cash flow visibility, reduces manual work, and ensures accurate financial records for your healthcare organization.
We're an AI-Powered Healthcare Claim Management Software Development Company
Managing healthcare claims today needs more than digital tracking. It needs smart systems that speed up reimbursements, reduce denials, and ensure compliance. At Citrusbug Technolabs, we use our healthcare expertise and AI-driven engineering to build healthcare claim management software that works for providers, insurers, and administrators.
Our healthcare claims management software uses machine learning, natural language processing (NLP), and automation to check claims, find errors, and simplify approvals. This lowers administrative work. It also improves accuracy and transparency in payments.
The software connects easily with EHRs, billing systems, payer networks, and other healthcare IT tools. It is secure, scalable, and ready to grow with your organization.

Looking for the best healthcare claims management software development company in India & USA?
Connect with our skilled developers for expert guidance and tailored solutions that meet your unique healthcare claim processing needs.
Our Healthcare Claim Management Capabilities
Claims Integration
Integrate with EHRs, billing systems, and payer systems smoothly and easily. This ensures accurate data exchange, smooth claim submission, and faster processing across your entire healthcare ecosystem.
Claims Review Management
Utilize automated claim reviews using AI to validate guidelines. We help identify missing information, reduce errors, and improve approval rates, which means fewer denials and quicker payments.
Claims Reporting
Access interactive, real-time reports showing individual claim performance. Draw on rich insights to identify bottlenecks, manage KPIs, and be able to make better-informed financial and operational decisions.
Electronic Data Interchange (EDI)
Enable secure, compliant, and automated data exchange between providers and payers. With EDI support, we can help improve claim communication and reduce manual work while improving claim communication speed and accuracy.
Status Management
Monitor each claim at each level of the cycle. With real-time status updates, the frequency of follow-ups decreases, visibility improves, and providers gain greater control over reimbursements.
Remittance Management
Simplify remittance through automated payment posting and reconciliation. Improved accuracy in financial records, less manual effort and more insight into payment trends and outstanding claims.
How Much Does it Cost to Develop Healthcare Claims Management Software?
The cost of developing a healthcare claim management software can range anywhere from $30,000 for a basic version to over $350,000 for a feature-rich, enterprise-grade solution.
Since every project depends on features, integrations, and compliance needs, share your requirements with us to get an exact estimate tailored to your idea.
Our Healthcare Claim Management Software Ensures Full Regulatory Compliance
Data security and compliance are at the core of every claims management solution we design. All of our software is built to the highest industry standards, ensuring that your organization is protected, compliant and audit-ready.
HIPAA
Protects sensitive health and financial information of patients using encryption and access controls to ensure compliance with healthcare privacy regulations at all times.
HITECH Act
Supports secure handling of digital health data while promoting interoperability and meaningful use, ensuring claims processes meet federal compliance requirements effectively.
GDPR
Ensures proper handling of patient and financial data for EU-related operations, maintaining transparency, accountability, and strict privacy protection across all workflows.
HL7 & FHIR Standards
Facilitates secure, structured data exchange between healthcare IT systems, improving interoperability and streamlining claim workflows across providers, payers, and administrators efficiently.
SOC 2 Standards
Implements strong security, availability, and confidentiality practices, ensuring your claim management software follows industry-leading standards for data safety and reliability.

Our Technology Stack for Healthcare Claim Management Platform
-
AI & Machine Learning
Automates claim validation, reduces denials, and provides predictive insights to ensure reimbursement is both accurate and efficient.
-
Natural Language Processing (NLP)
Simplifies claim documentation and coding by extracting relevant information quickly and accurately from unstructured data.
-
Cloud Infrastructure
Ensures scalable, reliable, compliant hosting to provide accessibility to healthcare organizations of all sizes.
-
APIs & System Integrations
Connects with EHRs, billing, and payer systems to streamline claim workflows and enable smooth interoperability.
Our Healthcare Claims Management System Development Process

We begin by understanding your healthcare organization’s workflows, claim handling challenges, and compliance requirements. Through extensive research and analysis, we develop a clear plan to create your custom claim management solution.

We design intuitive and user-friendly interfaces for healthcare providers, payors, and administrators. Our designs are geared to simplify complex claim processes and ensure compliance with regulations and accessibility.

We build custom healthcare claims management software that is built and secured using modern technologies and standards, which aligns with recommended frameworks. Each feature is designed and built to increase efficiency in our processes and improve claim processing accuracy.

We follow an iterative approach to ensure smooth deployment and continuous optimization. Our team delivers a reliable solution that adapts to your evolving healthcare claim processing needs.

Why Choose Citrusbug as Your Healthcare Claim Management Software Development Agency?
Our healthcare claim management software development company is rated 4.7 on Clutch with 30+ client reviews, and we’re a top rated plus agency on Upwork. We proudly maintain a 97% job success rate and have successfully delivered 500+ projects, showcasing our commitment to quality, reliability, and client satisfaction.

Transparency & Integrity
We safeguard your healthcare claim management ideas with strict NDA practices and ensure complete transparency throughout the development process. Your vision stays protected and executed with integrity.

On-Time Delivery
To ensure you receive your claim management software on time, our developers strictly adhere to a clear road map and timetable. By utilizing our claim management software, you can get your operations streamlined without waiting

Cost-Efficient
We combine quality with competitive prices by providing quality healthcare claim management solutions at low prices, giving you real value for your investment.

Deep Technical Knowledge
With years of expertise in building healthcare applications, our developers bring advanced technical knowledge to create secure, scalable, and compliant claim management systems.

QA and Testing
Our QA specialists perform detailed testing to ensure your healthcare claims management software is error-free, reliable, and fully ready for real-world deployment.

24X7 Availability
Resolve all your queries by contacting our experts 24X7. You can easily connect with us via text, email, Skype, or call whenever you need assistance.
Client Testimonials (We're Rated 4.7 on Clutch)
AI-focused Healthcare Software Projects We’ve Delivered
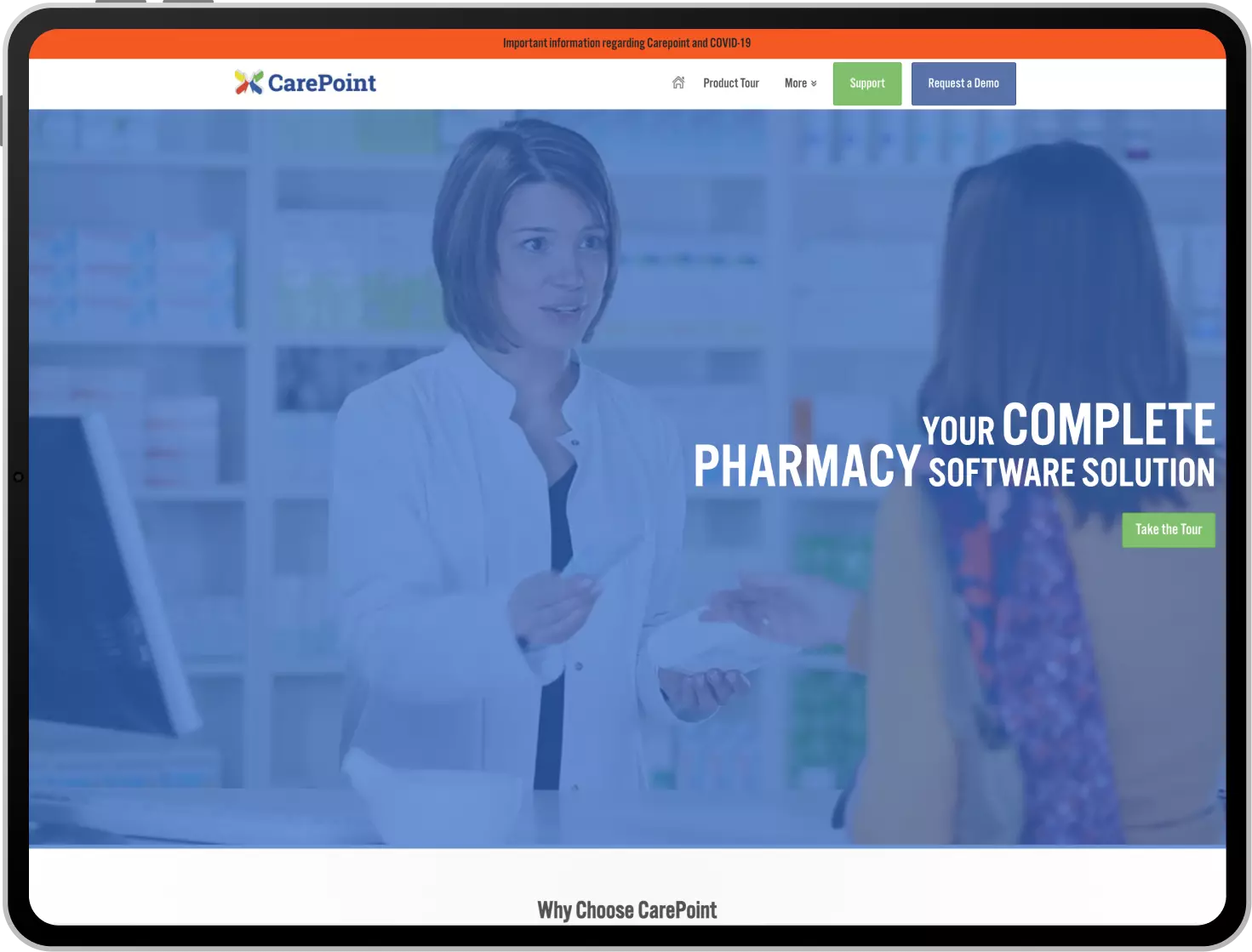
Carepoint is a solution dedicated to the pharmacy industry with a variety of tools needed to manage any pharmacy. This pharmacy management solution also offers integral support to manage dispensing, medication therapy, compounding support, A/R & reconciliation, and perpetual inventory.
Furthermore, this tool provides the ability to manage different virtual or real inventories with minimum effort. This platform also offers a range of customization for flexibility for any individual pharmacy. Users can make the most out of this tool and resolve any of the challenges that they generally face.
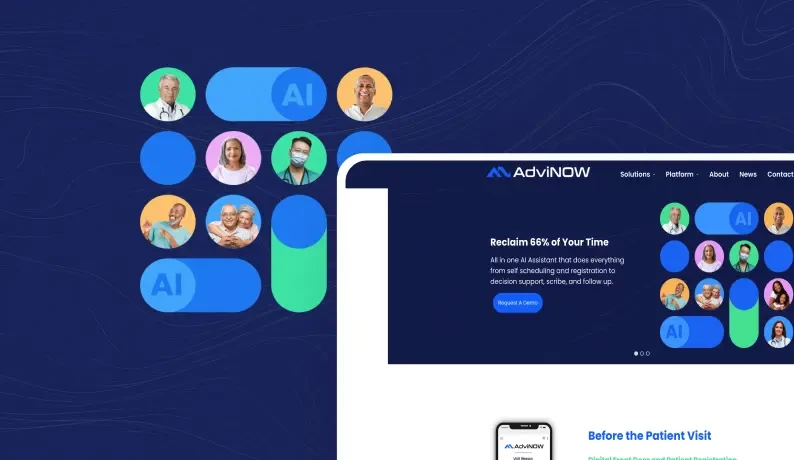
Advinow is an AI-driven healthcare platform that automates patient engagement and consultation processes, helping healthcare providers deliver efficient, on-demand services while improving operations for urgent care.
Droice Labs is a middleware designed to transform messy, unstructured patient data into clean, analysis-ready formats for clinical trials. Ensuring HIPAA/GDPR compliance, the platform automates data processing from EHRs, labs, and claims, providing scalable and high-quality regulatory-compliant insights.
Phelix is a no-code, virtual assistant designed for healthcare workflows by automating patient communication, scheduling, and payment processes. With advanced AI features like OCR, generative AI, chatbot functionality, and SMS automation, Phelix enhances efficiency, reduces administrative burden, and ensures good patient experiences. Phelix supports over 31 million patients across Canada and helps healthcare providers to focus on delivering quality care.

Latest Insights on Healthcare AI Software Development
FAQs on Healthcare Claims Management Software
Healthcare claims management is the process of preparing, submitting, and tracking medical claims. This process connects providers to patients and their insurance to provide accurate reimbursement while reducing administrative burden, errors and delays.
Insurance and healthcare organizations use healthcare claims management software to manage claims electronically. These platforms automate processes such as validation, coding, submission, and reporting to improve revenue cycle management and automate workflows.
A basic claim management software starts from $40,000-$60,000, while a mid-level claim management system, which includes some automation and payer integration, ranges between $100,000-$180,000. A software with advanced features like AI analytics can start from $250,000 or even higher.
Developing a healthcare claim management system typically takes 4 to 6 months. But it can be different based on your feature, integration and compliance requirements.
By utilizing natural language processing (NLP) and machine learning, our solution pulls critical information from unstructured data on the fly to automate coding and documentation. As a result, utilization can reduce manual effort and be more accurate.
Yes! We strictly comply with regulatory compliance standards that center on patient data and financial data, no matter where you practice, in the U.S., E.U., or beyond.




 SaaS Development
SaaS Development Web Application Development
Web Application Development Mobile Application Development
Mobile Application Development Custom Software Development
Custom Software Development Cloud Development
Cloud Development DevOps Development
DevOps Development MVP Development
MVP Development Digital Product Development
Digital Product Development Hire Chatbot Developers
Hire Chatbot Developers Hire Python Developers
Hire Python Developers Hire Django Developers
Hire Django Developers Hire ReactJS Developers
Hire ReactJS Developers Hire AngularJS Developers
Hire AngularJS Developers Hire VueJS Developers
Hire VueJS Developers Hire Full Stack Developers
Hire Full Stack Developers Hire Back End Developers
Hire Back End Developers Hire Front End Developers
Hire Front End Developers AI Healthcare Software Development & Consulting
AI Healthcare Software Development & Consulting Healthcare App Development
Healthcare App Development EHR Software Development
EHR Software Development Healthcare AI Chatbot Development
Healthcare AI Chatbot Development Telemedicine App Development Company
Telemedicine App Development Company Medical Billing Software Development
Medical Billing Software Development Fitness App Development
Fitness App Development RPM Software Development
RPM Software Development Medicine Delivery App Development
Medicine Delivery App Development Medical Device Software Development
Medical Device Software Development Patient Engagement Software Solutions
Patient Engagement Software Solutions Mental Health App Development
Mental Health App Development Healthcare IT Consulting
Healthcare IT Consulting Healthcare CRM Software Development
Healthcare CRM Software Development Healthcare IT Managed Services
Healthcare IT Managed Services Healthcare Software Testing services
Healthcare Software Testing services Medical Practice Management Software
Medical Practice Management Software Outsourcing Healthcare IT Services
Outsourcing Healthcare IT Services IoT Solutions for Healthcare
IoT Solutions for Healthcare Medical Image Analysis Software Development Services
Medical Image Analysis Software Development Services Lending Software Development Services
Lending Software Development Services Payment Gateway Software Development
Payment Gateway Software Development Accounting Software Development
Accounting Software Development AI-Driven Banking App Development
AI-Driven Banking App Development Insurance Software Development
Insurance Software Development Finance Software Development
Finance Software Development Loan Management Software Development
Loan Management Software Development Decentralized Finance Development Services
Decentralized Finance Development Services eWallet App Development
eWallet App Development Payment App Development
Payment App Development Money Transfer App Development
Money Transfer App Development Mortgage Software Development
Mortgage Software Development Insurance Fraud Detection Software Development
Insurance Fraud Detection Software Development Wealth Management Software Development
Wealth Management Software Development Cryptocurrency Exchange Platform Development
Cryptocurrency Exchange Platform Development Neobank App Development
Neobank App Development Stock Trading App Development
Stock Trading App Development AML software Development
AML software Development Web3 Wallet Development
Web3 Wallet Development Robo-Advisor App Development
Robo-Advisor App Development Supply Chain Management Software Development
Supply Chain Management Software Development Fleet Management Software Development
Fleet Management Software Development Warehouse Management Software Development
Warehouse Management Software Development LMS Development
LMS Development Education App Development
Education App Development Inventory Management Software Development
Inventory Management Software Development Property Management Software Development
Property Management Software Development Real Estate CRM Software Development
Real Estate CRM Software Development Real Estate Document Management Software
Real Estate Document Management Software Construction App Development
Construction App Development Construction ERP Software Development
Construction ERP Software Development



















 BOOK A 30 MIN CALL
BOOK A 30 MIN CALL