Billing Software for Mental Health Professionals: Key Features and Strategic Benefits
- September 25, 2025
-
743 Views
- by Ishan Vyas
Table of Contents
- Why Mental Health Professionals Struggle with Billing
- What is Billing Software for Mental Health Professionals?
- Key Features of Billing Software
- Strategic Benefits of Using Billing Software
- How AI Enhances Billing Software
- How to Choose the Right Billing Software for Mental Health Practices?
- Future Trends in Mental Health Billing Software
- Conclusion
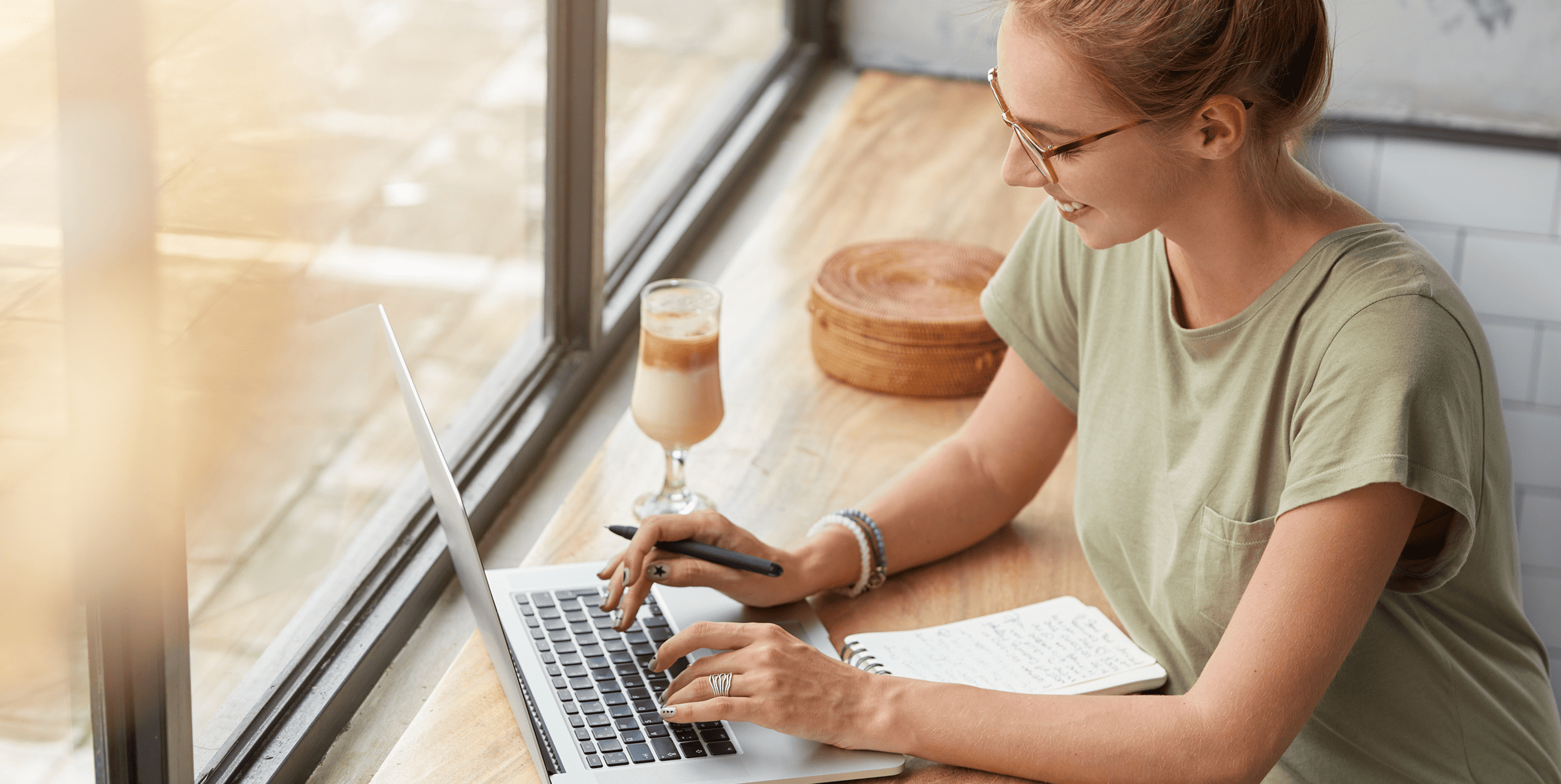
Billing is one of the most difficult aspects of being a therapist or running a mental health clinic. Whether it’s managing insurance claims or dealing with compliance requirements, the process can feel daunting and draining. Many providers now rely on billing software for mental health professionals to ease these frustrations and gain better control over their revenue cycle.
The proper solution encompasses much more than just invoice creation. It organizes claims submissions, minimizes errors that delay payments, and frees up clinicians to spend more time with patients and less time on administrative work. In this blog, we will discuss the important aspects and strategic benefits of billing software for mental health professionals.
Why Mental Health Professionals Struggle with Billing
One of the most frustrating aspects of running a mental health practice is billing. Insurance claims, adherence to regulations, and the routine implementation of administrative duties occupy both time and energy that could be used to treat patients.
Some of the most significant challenges are as follows:
- Complex insurance claims – Any mistake in the coding or incomplete record would lead to denials.
- Compliance pressures – HIPAA and other laws have to be adhered to secure confidential information about patients.
- Manual work in billing – It can take hours per week to manually enter session data, update invoices and follow up on co-pays.
- Integration gaps – When billing software does not connect to EHR or scheduling tools, information needs to be added several times, which enhances errors.
- Delayed payments – Rejected or slow claims are affecting the cash flow and complicating the financial planning.
These are some of the problems that can overwhelm even experienced staff in billing. A clear understanding of the problem areas is the first step to finding the solutions, which will save time and stress.
What is Billing Software for Mental Health Professionals?
Billing software for mental health professionals is created to manage the financial activity of a practice more effectively. It handles operations like the filing of insurance claims, monitoring of co-payments, creation of invoices and ensuring that it is in line with HIPAA and other laws. They are designed to assist therapists, counselors and mental health clinics in solving issues such as claim denials, coding mistakes, and administrative bottlenecks.
These solutions usually support electronic health records, appointment scheduling, and other practice management systems, unlike general medical billing tools. This saves on duplication of data entry, minimizes errors, and ensures accurate records. The solutions developed using strong EHR software development principles provide a smooth integration with patient records and workflows.
The software enables clinicians and staff to spend more time attending to the patients instead of completing the administrative duties by simplifying the billing procedures. It also gives a clear description of financial operations and helps to make better decisions and minimize the stress that comes with billing management.
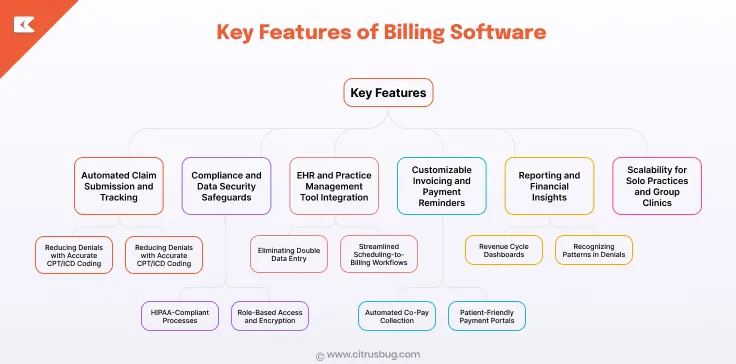
Key Features of Billing Software
Automated Claim Submission and Tracking
-
Reducing Denials with Accurate CPT/ICD Coding
Correct coding with CPT and ICD is essential for a successful claim submission process. Using this feature reduces claim denials by automatically validating codes against insurance requirements, saving staff significant time and administrative burden.
-
Real-Time Claim Status Updates
Real-time claims status updates keep staff informed of the status of each claim. Knowing where a claim is in processing enables billing teams to address issues, follow up on pending claims, and avoid delays in reimbursement.
Compliance and Data Security Safeguards
-
HIPAA-Compliant Processes
HIPAA-compliant processes ensure patient data is securely maintained throughout the billing process. These processes protect patient confidentiality, mitigate the risk of violations, and assist with regulatory compliance to build employee and patient confidence in the system.
-
Role-Based Access and Encryption
Role-based access protects sensitive information and limits access to healthcare personnel only, while encryption protects data from unauthorized parties. Collectively, these protections provide security and reduce the risk of breach or accidental disclosure of information.
EHR and Practice Management Tool Integration
-
Eliminating Double Data Entry
Linking to electronic health records and scheduling systems facilitates the removal of repetitive actions to enter patient data. This minimizes mistakes, wastage of time and makes sure that there is consistency in all records within the practice.
-
Streamlined Scheduling-to-Billing Workflows
When appointments are integrated directly into billing, this simplifies the scheduling-to-billing workflow. This guarantees correct billing of each session, reduced missed bills, and better revenue management. The EHR software development is commonly used to improve the integration process and guarantee the smooth flow of data and the dependability of the system.
Customizable Invoicing and Payment Reminders
-
Automated Co-Pay Collection
Automated co-pay collection enables practices to get payments on time without necessarily having to follow up manually. It gives the staff more time to concentrate on other administrative processes and it also provides the patients with a more convenient payment procedure.
-
Patient-Friendly Payment Portals
Patient portals make it simple to view and pay invoices online. This not only drives transparency into the payment experience to lessen missed payments, but it also helps practices create uninterrupted cash flow.
Reporting and Financial Insights
-
Revenue Cycle Dashboards
Revenue cycle dashboards provide a clear picture of the financial performance of the practice among the staff. Visualizing claims, payments, and outstanding invoices helps teams assess performance and make informed decisions.
-
Recognizing Patterns in Denials
The ultimate analysis of denied claims provides patterns that can reflect repetitive problems. These patterns can be tackled to enhance the approval ratios and the optimization of revenue over the years.
Scalability for Solo Practices and Group Clinics
Modern billing software is built to scale to the practice. Whether accommodating a solo practitioner or a multi-provider clinic, these solutions can accommodate increased claim volume, manage multiple locations, and generate more patient records while maintaining efficiency.
Strategic Benefits of Using Billing Software
Streamlined Operations and Time Savings
The billing software makes it possible to automate routine activities like creating invoices, payment reminders, and claim tracking. The administrative work is not as extensive that the staff is not overly overworked and clinicians are able to better utilize the time they have to care and the running of the practice is much easier and efficient.
Improved Revenue and Financial Oversight
Practices have better cash flow and financial stability with accurate claims and quicker reimbursements. The visibility on the pending claims and payments can assist staff members in managing more budgets and making decisions with less additional administrative effort.
Enhanced Compliance and Risk Reduction
HIPAA-compliant workflows and role-based access ensure sensitive patient data is protected. This minimizes chances of error or breaches and it assists practices to always be up to standard on the regulatory requirements and this gives clinicians and patients confidence in the system.
Growing Practice Scalability
The billing software may be expanded with the practice, accommodating solo practitioners, multi-provider clinics, and multiple sites. It can support higher volumes of patients and more complicated workflows without introducing an operational burden, and it is appropriate to support the long-term expansion of practices.
Data-Driven Insights for Better Decisions
Analytics and reporting provide actionable insights into payment trends, denied claims, and operational efficiency. These insights help optimize operations, and integration with healthcare claim management software can provide automated recommendations for improved performance.
How AI Enhances Billing Software
Smarter Claim Processing
- Predicts potential issues in claims to reduce rejections.
- Ensures faster reimbursements by prioritizing high-risk claims.
- Frees staff from manually reviewing every submission.
Improved Accuracy and Error Reduction
- Detects inconsistencies or missing billing information automatically.
- Minimizes coding errors that cause payment delays.
- Continuously learns from real-world claim data through AI in EHR.
Enhanced Patient Engagement
- Conversational AI answers billing questions and sends reminders.
- Reduces staff workload while providing faster patient support.
- Improves patient satisfaction through personalized assistance.
Workflow Automation and Efficiency
- Automates follow-ups on outstanding claims and the generation of reports.
- Eases the payment reconciliation and financial tracking.
- Ensures productivity despite the increasing number of patients.
Scalable and Adaptive Systems
- Learns and adapts to handle increasing claim complexity.
- Supports more providers and patients without adding manual effort.
- Uses generative AI for healthcare to enhance workflow intelligence over time.
How to Choose the Right Billing Software for Mental Health Practices?
When selecting billing software for mental health practices, the following factors should be kept in mind to save costs and maintain a competitive edge.
1. Ease of Use
The software must be user-friendly with a minimized learning curve for the staff and clinicians. An easy-to-use, well-structured design will reduce errors in submitting claims and invoicing and enable the staff to spend more time on patient care and day-to-day activities.
2. Integration Capabilities
Integration with the EHR, scheduling and practice management systems is essential. This guarantees proper patient documentation, avoids data repetition, and maintains work processes. It also enables future upgrades of practices without interfering with the current processes.
3. Compliance and Security
This is necessary to protect sensitive patient information. The appropriate software facilitates HIPAA-compliant operations, role-based access controls, and secure data storage that decreases chances of breach or regulatory fines and still builds trust with patients.
4. Scalability and Flexibility
The billing programs have to expand along with the practice. It must have the capacity to manage increased patient volumes and more complex workflows without increasing operational burden, whether using solo practitioners or multi-provider clinics. The ability to customize features means that the system is flexible to changing practice requirements.
5. Cost Considerations
The cost to develop billing software for mental health generally ranges from $20,000 for basic software and goes upto $250,000 for software with advanced features. Considering cost before investing in custom software development avoids surprises in the future.
6. Analytics and Reporting
Modern healthcare software provides insights into revenue trends, denied claims, and workflow efficiency. These analytics allow staff to make informed, data-driven decisions and optimize the revenue cycle. Predictive tools or dashboards can further support long-term financial planning.
7. Customization for Mental Health Practices
Mental health workflow-specific software has the potential to automate reminders, co-pay collection and reporting. Custom solutions, enhanced through medical billing software development, ensure accuracy and efficiency, aligning perfectly with the unique needs of mental health clinics.
Future Trends in Mental Health Billing Software
AI-Powered Automation
AI is increasingly automating claim processing, coding, and error detection. This decreases denials of claims by 25-30 percent and speeds up the processes of reimbursements while machine learning applications keep up with the changing insurance regulations.
Telehealth Reimbursement Growth
Medicare has permanently expanded telehealth coverage for behavioral health, including audio-only visits. This ensures broader access to virtual care and standardized reimbursement rates, supporting clinics in offering flexible treatment options.
Integration of Digital Therapeutics
FDA-cleared digital therapeutic apps are increasingly reimbursed through new CMS HCPCS codes. Providers can bill for software-based therapies integrated into patient care plans, promoting innovation in mental health treatment.
Focus on Compliance and Security
Computerized invoicing programs are improving HIPAA regulations and maximizing the accuracy of codes. Clinics can avoid the risk of fraud and comply with the regulations by minimizing human errors and ensuring the safety of patient records.
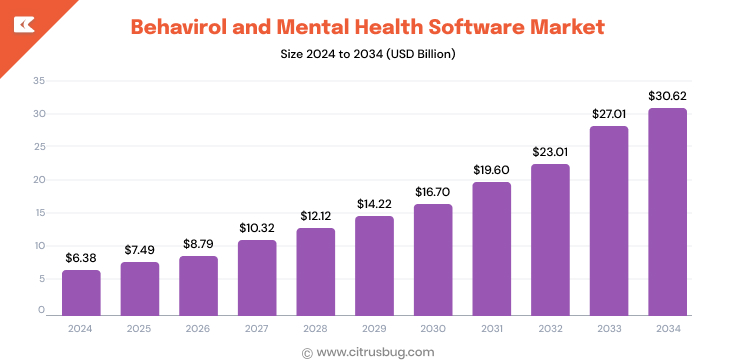
Behavioral Health Software Market Growth
The global behavioral and mental health software market is projected to grow from USD 7.49 billion in 2025 to USD 30.62 billion by 2034, at a CAGR of 16.98%. This growth is fueled by increasing mental health awareness, supportive policies, and widespread adoption of cloud-based solutions.
Conclusion
Mental health practice billing software is rapidly advancing and provides the capability to make the process of claiming easier, more compliant, and to provide better financial information. The adoption of AI-enabled tools and predictive analytics is assisting medical practices in making fewer mistakes, accelerating payment procedures, and spending more time with the patients.
Partnering with a medical billing software development company can help organizations implement customized solutions that fit into their workflows. Citrusbug’s deep technical expertises make sure that businesses can maximize revenue cycles, maintain compliance and scale efficiency as their business grows.




 SaaS Development
SaaS Development Web Application Development
Web Application Development Mobile Application Development
Mobile Application Development Custom Software Development
Custom Software Development Cloud Development
Cloud Development DevOps Development
DevOps Development MVP Development
MVP Development Digital Product Development
Digital Product Development Hire Chatbot Developers
Hire Chatbot Developers Hire Python Developers
Hire Python Developers Hire Django Developers
Hire Django Developers Hire ReactJS Developers
Hire ReactJS Developers Hire AngularJS Developers
Hire AngularJS Developers Hire VueJS Developers
Hire VueJS Developers Hire Full Stack Developers
Hire Full Stack Developers Hire Back End Developers
Hire Back End Developers Hire Front End Developers
Hire Front End Developers AI Healthcare Software Development & Consulting
AI Healthcare Software Development & Consulting Healthcare App Development
Healthcare App Development EHR Software Development
EHR Software Development Healthcare AI Chatbot Development
Healthcare AI Chatbot Development Telemedicine App Development Company
Telemedicine App Development Company Medical Billing Software Development
Medical Billing Software Development Fitness App Development
Fitness App Development RPM Software Development
RPM Software Development Medicine Delivery App Development
Medicine Delivery App Development Medical Device Software Development
Medical Device Software Development Patient Engagement Software Solutions
Patient Engagement Software Solutions Mental Health App Development
Mental Health App Development Healthcare IT Consulting
Healthcare IT Consulting Healthcare CRM Software Development
Healthcare CRM Software Development Healthcare IT Managed Services
Healthcare IT Managed Services Healthcare Software Testing services
Healthcare Software Testing services Medical Practice Management Software
Medical Practice Management Software Outsourcing Healthcare IT Services
Outsourcing Healthcare IT Services IoT Solutions for Healthcare
IoT Solutions for Healthcare Medical Image Analysis Software Development Services
Medical Image Analysis Software Development Services Lending Software Development Services
Lending Software Development Services Payment Gateway Software Development
Payment Gateway Software Development Accounting Software Development
Accounting Software Development AI-Driven Banking App Development
AI-Driven Banking App Development Insurance Software Development
Insurance Software Development Finance Software Development
Finance Software Development Loan Management Software Development
Loan Management Software Development Decentralized Finance Development Services
Decentralized Finance Development Services eWallet App Development
eWallet App Development Payment App Development
Payment App Development Money Transfer App Development
Money Transfer App Development Mortgage Software Development
Mortgage Software Development Insurance Fraud Detection Software Development
Insurance Fraud Detection Software Development Wealth Management Software Development
Wealth Management Software Development Cryptocurrency Exchange Platform Development
Cryptocurrency Exchange Platform Development Neobank App Development
Neobank App Development Stock Trading App Development
Stock Trading App Development AML software Development
AML software Development Web3 Wallet Development
Web3 Wallet Development Robo-Advisor App Development
Robo-Advisor App Development Supply Chain Management Software Development
Supply Chain Management Software Development Fleet Management Software Development
Fleet Management Software Development Warehouse Management Software Development
Warehouse Management Software Development LMS Development
LMS Development Education App Development
Education App Development Inventory Management Software Development
Inventory Management Software Development Property Management Software Development
Property Management Software Development Real Estate CRM Software Development
Real Estate CRM Software Development Real Estate Document Management Software
Real Estate Document Management Software Construction App Development
Construction App Development Construction ERP Software Development
Construction ERP Software Development